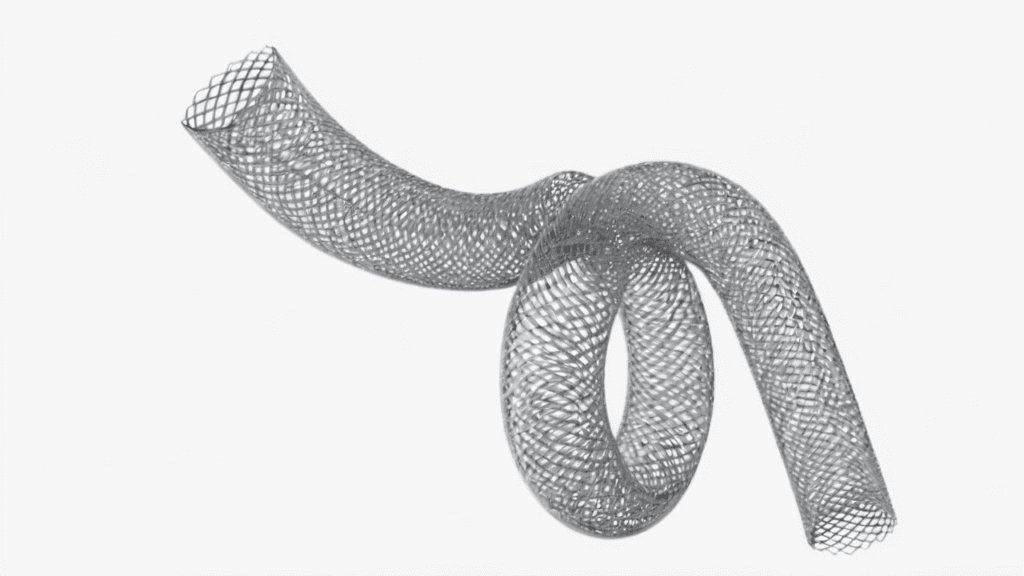
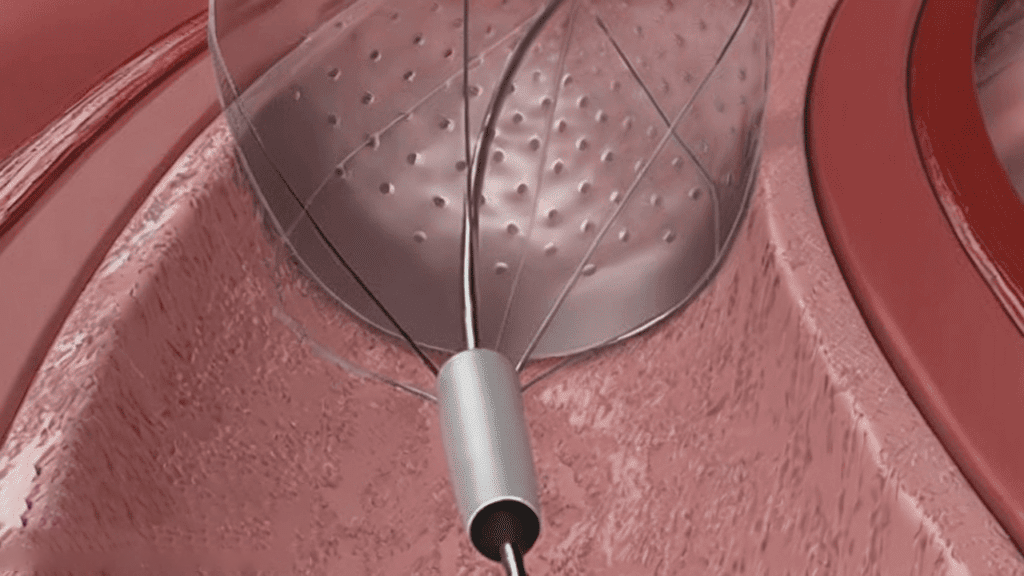
Flow diverters have transformed the treatment landscape for complex intracranial aneurysms, offering a minimally invasive approach to redirect blood flow and promote aneurysm healing. However, the effectiveness of these devices depends heavily on their surface properties. Specialized coatings are becoming essential for addressing clinical challenges, improving patient outcomes, and enhancing the safety and durability of these neurovascular devices.
This article explores recent advancements in flow diverter coatings and examines how these technologies impact neurovascular treatments, leading to better patient care and expanded treatment possibilities.
Why Coatings Matter in Flow Diverters
Flow diverters are typically crafted from durable alloys like cobalt-chromium and are designed to be placed across the neck of an aneurysm. By diverting blood flow away from the aneurysm sac, these devices facilitate vessel remodeling, gradually closing the aneurysm and promoting natural healing. However, bare metal flow diverters face several critical issues. Without proper surface treatment, they are prone to:
- Thrombosis
- Delayed endothelialization
- Inflammatory responses
These limitations often necessitate prolonged dual antiplatelet therapy (DAPT) to prevent clotting, which adds complexity to treatment and limits patient eligibility. This has driven the need for advanced coatings that optimize biocompatibility and performance in neurovascular applications.
Core Functional Goals of Flow Diverter Coatings
The best coatings address several key performance metrics:
| Reduce Thrombogenicity | By preventing platelet adhesion and activation, specialized coatings lower the risk of clot formation. |
|---|---|
| Minimize Inflammatory Responses | Reducing immune reactions enhances biocompatibility, supporting long-term device stability and integration with the vessel wall. |
| Promote Rapid Endothelialization | Coatings that support cellular adhesion help form a natural vessel lining over the device, creating a stable interface. |
| Potentially Reduce the Need for Long-Term DAPT | With lower thrombosis risk, coatings may help patients avoid prolonged DAPT, making treatments safer and more accessible for a broader range of patients. |
Overview of Innovative Coating Technologies
Hemocompatible Passive Coatings
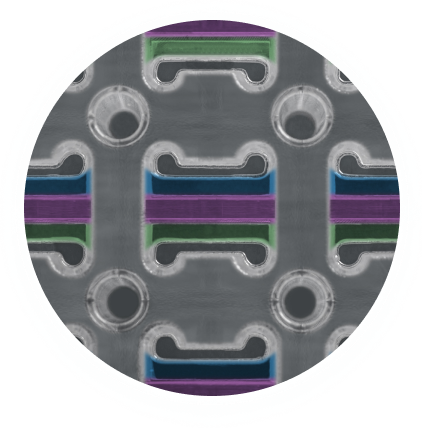
Smart Reactors’ Camouflage™ technology represents this approach. It uses a synthetic polymer and proteinaceous base to “camouflage” the device, shielding it from direct blood contact. This minimizes clot formation, supports endothelial cell growth, and improves healing without using pharmaceutical agents.
Bioactive Coatings
These coatings integrate growth factors or signaling molecules that actively encourage endothelial attachment and proliferation. The result is faster, more complete coverage by endothelial cells and improved integration with the vessel wall.
Heparin Coatings
Heparin-based technologies, such as CBAS, use known anticoagulant properties to minimize surface thrombosis. They facilitate faster endothelialization by maintaining a clean, thrombus-free surface and improving overall biocompatibility.
Clinical Impact: Improved Outcomes and Shorter Recovery
Studies have shown that flow diverters enhanced with specialized coatings can:
- Support shorter durations of dual antiplatelet therapy. These coatings optimize the healing process by supporting a smooth transition through the different phases of healing:
- Reduce thromboembolic complications by up to 50%
- Increase complete aneurysm occlusion rates at 6–12 months
These improvements are driven by a coating’s role during the:
Chronic Phase (3+ months): Advanced coatings continue to support ongoing endothelialization and device integration, ensuring long-term stability and compatibility with the vascular tissue.
Acute Phase (0–30 days): During the critical early days post-implantation, coatings provide immediate protection against thrombosis, reducing the risk of clot formation.
Subacute Phase (1–3 months): Coatings maintain stability as blood flow remodeling occurs, allowing endothelial cells to attach and cover the device’s surface, helping integrate it into the vessel wall.
The clinical benefits of these coatings make flow diverters safer and more suitable for high-risk patients, those with complex aneurysm structures, and patients unable to tolerate extended DAPT. As coatings facilitate quicker healing and improve compatibility, they expand the patient population that can benefit from these minimally invasive treatments.
Future Trends in Neurovascular Coating Innovation
Looking ahead, several promising innovations in flow diverter coatings could further advance neurovascular treatments. Smart, responsive coatings are being developed to adapt to changing physiological conditions, delivering antithrombotic agents or other therapeutic properties on demand. Bioresorbable coatings are also on the horizon, offering temporary benefits during critical healing phases before gradually degrading, leaving a fully integrated device. Additionally, combination therapy coatings are emerging, integrating multiple therapeutic functions (such as antithrombotic and anti-inflammatory effects) to achieve a synergistic impact on healing and biocompatibility.
Other future innovations include personalized coatings, which could be tailored to patient-specific factors, potentially based on genetic or biomarker data to enhance compatibility. Nanotechnology-enhanced coatings, designed to closely replicate natural vessel linings, offer further control over surface properties, creating biomimetic surfaces that improve device integration and reduce immune response.
Specialized coatings for flow diverters represent a pivotal advancement in treating complex aneurysms, offering a safer, more effective approach to neurovascular care. By reducing thrombosis, promoting endothelialization, and ensuring device stability, these coatings are enhancing the quality of life for patients undergoing neurovascular interventions. Technologies like Smart Reactors’ Camouflage™ are at the forefront of this evolution, delivering a hemocompatible, durable solution that meets the rigorous demands of modern neurovascular applications.
Frequently Asked Questions
How do hemocompatible coatings reduce the need for DAPT?
By reducing the risk of thrombosis at the device surface, hemocompatible coatings may allow patients to taper off antiplatelet therapy sooner under clinical supervision.
What is the difference between passive and bioactive coatings?
Passive coatings aim to minimize interaction with blood components, while bioactive coatings promote healing by stimulating endothelial cell behavior.
Are these coatings currently in clinical use?
Several are already integrated into commercial products. Smart Reactors’ Camouflage™ is an example of a passive hemocompatible coating undergoing validation for neurovascular applications.
Conclusion
Specialized coatings for flow diverters are elevating the safety, effectiveness, and accessibility of aneurysm treatment. By minimizing thrombosis, accelerating healing, and reducing the burden of antiplatelet therapy, these surface modifications are helping to broaden the range of patients who can benefit from minimally invasive neurovascular procedures.
Technologies like Smart Reactors’ Camouflage™ coating are leading the charge—offering a drug-free, hemocompatible solution that meets the demands of advanced neurovascular care.
As the field advances, coating innovation will remain central to improving outcomes for patients with some of the most challenging vascular conditions.
Share this post: on LinkedIn