Medical devices that come into contact with blood must be engineered for hemocompatibility — the ability to avoid triggering the body’s clotting and immune response. Poor hemocompatibility can result in thrombus formation on device surfaces, impairing function and creating downstream risks such as emboli, blocked vessels, and tissue damage.
Why Hemocompatibility Matters
Blood readily reacts to foreign materials. When exposed to a non-hemocompatible surface, platelets activate, fibrin forms, and clots begin to develop. These can:
Disrupt the function of implanted or extracorporeal devicesCompromise patient safetyLead to device failure or systemic complications
How Clots Form: Coagulation Pathways
When a device enters the bloodstream, it activates the intrinsic coagulation pathway. This is different from the extrinsic pathway, which is triggered by tissue injury. Key steps include:
- Plasma protein adsorption (e.g., fibrinogen, albumin — the Vroman effect)
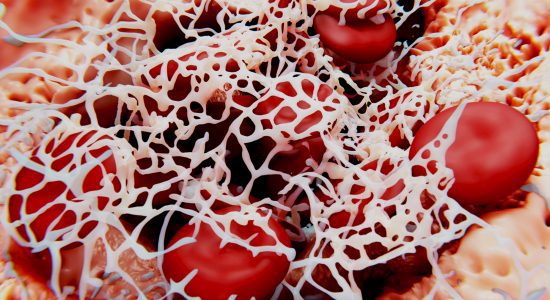
- Thrombin generation – a pivotal enzyme that converts fibrinogen to fibrin
- Fibrin mesh formation, trapping red cells and platelets
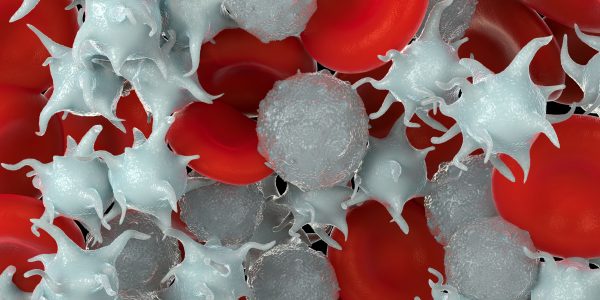
- Platelet activation, further amplifying the coagulation process
In parallel, white blood cells like neutrophils may release NETs (neutrophil extracellular traps), providing scaffolds for additional clotting activity.
Design Factors That Influence Hemocompatibility
Hemocompatibility is not just a material issue — it’s influenced by multiple device design variables:
| Design Element | Impact on Hemocompatibility |
| Material surface chemistry | Affects protein and platelet interactions |
| Geometry & flow dynamics | Can cause stagnation or turbulence that promotes clotting |
| Surface area and roughness | Larger or rougher areas increase activation risk |
| Duration of contact | Long-term implants have stricter requirements |
Microscale flow stagnation zones or areas of high shear can both elevate clot risk. Poorly optimized surfaces also raise the chance of hemolysis and immune activation.
Evaluating Hemocompatibility: Test Methods
The medical device design process needs to consider evaluating a device’s hemocompatibility at an early stage to ensure its ability to perform in blood is “designed in.” Various in-vitro and in-vivo tests have been developed that consider the complexity of the clotting cascade and the device’s surface/blood interactions.
The most common in-vitro assays rely on either static or dynamic blood contact. In-vitro dynamic testing produces the most detailed laboratory testing for evaluating a device’s performance without the cost, complexity, and ethical considerations of animal testing.
This testing can also be performed on individual materials and device sub-systems at a time when the entire device may not be ready for in-vivo evaluation, allowing developers to get an early indicator of device performance.
The table below shows some of the common test methods that are used and which cover the performance of a device with respect to the different mechanisms of clot initiation.
| Category | Test | Purpose | |
| Coagulation | Measurement of Thrombin-Antithrombin (TAT) complex using ELISA measurement | The purpose of the TAT Elisa assay is to determine the progression of sample blood towards coagulation as an indicator of the formation of fibrin networks. | |
| Hemolysis | The measurement of Free Hemoglobin by spectrophotometry | This measurement provides an indicator for how many erythrocytes are being lysed (freeing up hemoglobin). This tells how likely the device surface is to damage blood and lead to pro-coagulant constituents being released. | |
| Hematology | Measurement of circulating cell counts (Platelets, White Blood Cells, and Red Blood Cells) using commercial hematology analyzers | Reduction in circulating cell counts suggest that cells have either adsorbed on the surface or otherwise been incorporated into a blood clot. | |
| Platelet | Measurement of markers of platelet activation such as Beta-Thromboglobulin or Platelet Factor 4 using an ELISA Assay | The biological markers indicating platelet activation | |
| Complement | Measurement of complement activation markers such as C3a, C5a and SC5b9 using an ELISA assay | The activation of the complement system indicates an innate immune response to the surface of the device which can lead to coagulation | |
| Leukocyte Activation | Measurement of PMN Elastase using an ELISA Assay | The activation of PMN elastase indicates that there is an immune response mediated by leukocytes. | |
| Surface analysis | Microscopic Surface evaluation using SEM or light microscopy | The visual appearance of surfaces, particularly under SEM, can identify challenge areas and adherence of fibrin, platelets, and blood cells | |
Dynamic testing systems simulate realistic flow conditions and can be applied early in the design phase, before full prototypes are developed.
Improving Device Hemocompatibility with surface modification
Not all device materials are naturally blood-compatible. Materials like polypropylene or PMP often require surface enhancements to meet safety thresholds.
Camouflage™, Smart Reactors’ proprietary coating, helps solve this problem. It offers:
- Drug-free thromboresistance
- Reduced platelet adhesion
- Support for endothelialization
By modifying the device surface without altering mechanical performance, Camouflage™ enhances both short-term patency and long-term healing.
Why Surface Design Can’t Be Overlooked
Thrombus formation on blood-contacting medical devices is a preventable complication. Manufacturers must proactively design for hemocompatibility by considering:
- Material selection and surface chemistry
- Flow dynamics and geometry
- Surface coatings that reduce biological reactivity
At Smart Reactors, we support manufacturers through every phase of development — from prototype coatings to clinical-grade production — helping ensure their devices perform safely inside the body.
🔗 Explore Camouflage™ Coating Technology »
🔗 Read our vascular graft whitepaper »
Share this post: on LinkedIn